Surving Cancer: Does the Fighting Spirit Matter?
Inaugural Lecture, University of Hull, UK, 6th November 2000
Pro Vice-Chancellor, Members of Council, Members of Court, Ladies and Gentlemen. First of all, let me express my appreciation to all of you for coming to this Inaugural Lecture on such a wet night.
At the time of the French Revolution, there were two young men who had a problem. They both loved the same young lady. But, unfortunately, she was unwilling to say which she would like to marry. There was only one solution -in traditional time honoured fashion, a dual to the death at dawn in the Champs Élysées. The two suitors duly turned up; and so did a crowd from Paris. The contestants stood back to back and the referee handed each of them a pistol. Just as he was about to give starters orders, one of them shouted: 'Stop! This competition is inherently unfair.' Like me, he was well built, and his opponent was a small man indeed. He went on: 'I am twice as big a target as he is, so when we fire at each other, I should be twice as far away from him as he is from me!'
Well, the referee could see that there was some justice in what the big man was saying, but the solution was not obvious to him. However, the day was saved by a tailor who came forward from the crowd. He went up to the small man and, with his tailor's tape, measured the dimensions of the small man. Then he went up to the big man and, with his white tailor's chalk, marked off the outline of the small man. 'Now', he said, 'any bullets outside the white marks don't count!'
Surviving cancer: does the fighting spirit count? On which side of the chalk marks do psychosocial factors lie; inside or outside? Are psychosocial factors relevant to surviving cancer, or are they not? And, if they are relevant, how important are they, and how do they work?
My late father was a Church of Scotland Minister and, when I was a boy, he used to tell me that you should always say what you are going to say, then you should say it, and then you should say what you have said! So, in deference to my father, here is an overview of what I want to say tonight.
After a brief introduction about cancer, I shall discuss the impact of the diagnosis and treatment on the patient and the family. I shall then try to answer several questions. Can we prevent distress following the diagnosis? Can we improve quality of life? What are the implications of our own research findings, and those of others, in terms of the delivery and organisation of cancer services within the reformed National Health Service? Finally, can psychological interventions enhance survival and, if so, under what circumstances, and by which mechanisms?
The Impact of the Diagnosis and Treatment
So let's start at the beginning. What is the impact of the diagnosis and treatment of cancer? What is it like to be told you have cancer? What are the implications? One of my former patients from Aberdeen talks about her experience.
And then, still reeling from the diagnosis, there are usually treatments to be faced - treatments such as surgery, radiotherapy, hormone therapy and chemotherapy. My former patient from Aberdeen again.
It is not surprising, therefore, that the diagnosis and treatment of cancer are often associated with distress of various types, for example anxiety, depression, sexual problems, nausea, vomiting, fatigue, body image problems, pain and, what I like to call, the 'Damocles syndrome'. Patients with the Damocles syndrome become locked in the future, unable to enjoy the present for fear of recurrent disease.
Given these considerations, it is hardly surprising that well-conducted studies throughout the world have fairly consistently indicated high levels of psychiatric morbidity in patients following the diagnosis. In one of the early studies carried out in North America, 215 patients with different types and stages of cancer were assessed. Almost one in every two (47%) suffered from a diagnosable psychiatric disorder (Derogatis, Morrow, Fetting, et al., 1983).
Nearer to home at the Christie Hospital in Manchester, Professor Peter Maguire and his colleagues followed up a cohort of women for a year following breast surgery. They found that 25% of the women suffered from clinically significant anxiety and/or depression and 33% had moderate or severe sexual problems (Maguire, Lee, Bevington, et al., 1978). Even more strikingly, the same group found that no fewer than 81% of women receiving adjuvant combination chemotherapy for breast cancer developed a psychiatric disorder (Maguire, Tait, Brooke, et al., 1980).
Now these figures are alarming and distressing to say the very least of it. But what about the partners of patients with cancer? Cancer not only affects individuals; it also affects families. How do they cope?
One of the last studies that we carried out in Aberdeen before coming to Kingston-upon-Hull addressed the issue of the mental health of partners (Anderson, Walker & Walker, 2000). We found that, at diagnosis, the distress level was significantly higher in partners of women with breast cancer than it was in the patients themselves. As we followed up these women and their partners over a period of 24 weeks after the diagnosis, we found that distress levels very closely followed each other. In other words, a decrease in the distress level of one of the dyad was likely to be followed by a decrease in the distress level of the other. There may be an important therapeutic message here: by helping partners, we may be able to help patients.
Are these horrendous statistics inevitable? Can we do anything to improve them? Let's go back to basics. Let's think about the factors that predict psychological and psychiatric morbidity.
In a very useful paper, Harrison and Maguire (1994) reviewed predictors of psychological and psychiatric disorders in patients with cancer. They concluded that the following are risk factors: a previous history of mood disturbance, high emotionality, low ego strength, poor performance status ('fitness'), certain types of treatments (e.g. colostomy), lack of social support, passive or avoidant coping, inadequate or inappropriate information, and communication problems. To this we might add the number of unresolved concerns (Worden and Weisman, 1984) and the partner's distress level (Anderson, Walker & Walker, 2000).
Several of these predictors, such as a history of mood disturbance and performance status, cannot be altered. However, at least potentially, a number of these risk factors can be altered, for example ego strength, coping style, extent of the partner's distress, amount of support, number of unresolved concerns, adequacy of information, and satisfaction with communication.
With reference to satisfaction with communication, the next slide is adapted from a cartoon that I found in The Lancet. It is almost three quarters of a century old. The doctor is sitting behind his desk, scarcely looking at the patient -an example of how not to conduct a medical consultation. He says to the patient: 'You must give up your cocktails, your night-clubs and your smoking.' The women indignantly replies: 'But doctor, I don't do any of these things.' Untrammelled by her protestation, the doctor presses on: 'Well, in that case, I will give you a prescription to help with your memory loss!' Hardly a recipe for empathic communication and compliance with treatment!
I have tried to bring that cartoon up to date in the next two slides, and also to take some of the heat off health care professionals. Communication between husband and wife is important too. Having examined the patient, the doctor says to her: 'You must drink plenty fluids, keep warm and make sure that you bathe your skin regularly.' The patient then goes outside and speaks to her husband, who asks her what the doctor said. The wife replies: 'He said that I must have a regular supply of fine wine, a constant supply of new designer outfits and regular beach holidays in the Caribbean!' Poetic licence is cast in a new light!
We were first alerted to the importance of information and communication in our early studies in the Granite City (Paraskevaidis, Kitchener & Walker, 1993). We followed up 118 women who had been treated previously for gynaecological cancer. Most patients were doing very well clinically; their disease was in remission. We found that those who had clinically significant anxiety and depression were much more likely to be dissatisfied with the relationships that they had with the hospital doctors and were more likely to have been less satisfied with the information they received following the diagnosis.
Now this sounds a rather negative conclusion, but it need not be. We can turn it into a positive conclusion. Perhaps we can prevent distress and morbidity by improving satisfaction with communication, and by making sure that the information we give is the information that is going to assist and enable the patient to cope (Walker, 1996).
We do well to remember the wise words of T S Eliot, when he distinguished wisdom, knowledge and information:
Where is the life we have lost in living?
Where is the wisdom we have lost in knowledge?
Where is the knowledge we have lost in information?
There is a view in the NHS at the moment that, if only we can give patients more, and more, information, then all the problems of coping with the diagnosis and treatment will be solved. I believe that view to be both naïve and misguided. Of course accurate information can be vitally enabling; but information given at the wrong time, in the wrong way, or by the wrong person can be very damaging to patients, and their relatives. In our study of women with gynaecological cancer, although many said they would have coped better with more information, there was a small subgroup who believed they would have coped better with less information (Paraskevaidis, Kitchener & Walker, 1993). That is why there is a need for communication skills training for all health professionals, during basic training and afterwards (Klein, Kitchener, Tracy, et al., 2000; Walker, 1996).
Prevention Better than Cure
With these considerations about risk factors in mind, ten years ago in Aberdeen we designed a service that we hoped would minimise distress and improve quality of life. The result was a Behavioural Oncology Unit that included a 'drop-in' centre that was fully integrated functionally, and physically, with the medical and surgical oncology services.
We cultivated a professional but informal atmosphere -the kettle was always on. Patients and their relatives were welcome to visit or telephone at any time. We gave our staff special training to make sure that they had the skills necessary to elicit cancer-related concerns and, equally importantly, to respond effectively to these. We customised the information given. We provided the opportunity for peer group and staff support. And, as far as patients were concerned, psychosocial support and medical and surgical treatment were seamlessly integrated. Psychosocial support was not like a sunroof in a car; it was not an add-on extra. The Unit was physically a part of the Professorial Surgical Unit and patients received their chemotherapy under the supervision of a consultant medical oncologist within the Behavioural Oncology Unit. It was possible for us to make sure that, from the patient's point of view, investigations and treatments were carried out with the minimum delay; the minimum fuss, and the maximum co-ordination. I am delighted that my friend and colleague Professor Oleg Eremin, the former Regius Professor of Surgery at the University of Aberdeen, who did so much to promote Behavioural Oncology in Aberdeen, is in the audience tonight.
In one of our studies, 96 women attending the Unit because of newly diagnosed locally advanced breast cancer were studied intensively over a period of 37 weeks (Walker, Walker, Ogston, et al., 1999). They were assessed using a number of tests, including the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983). Immediately after the diagnosis had been made, when they were in-patients in the Professorial Surgical Unit, waiting to start their chemotherapy, 21% scored 11 or above on the anxiety sub-scale of the HADS. This is usually taken to indicate clinically significant anxiety. However, the figure of 21% is not very interesting. We had carried out surveys of other groups of women in the North East of Scotland, for example surveys of female polices officer, female psychiatric nurses and wives of police officers. We had consistently found a point prevalence of 15-25% in community samples. These women with newly diagnosed breast cancer were undoubtedly stressed; but they were not clinically dis-stressed.
Eighteen weeks later, having had six cycles of chemotherapy and whilst awaiting surgery, the point prevalence had fallen to 5%. This is obviously much lower than it had been at diagnosis, and much lower than it was in the so-called healthy population of the Granite City and its environs.
Thirty-seven weeks after the diagnosis, following chemotherapy, surgery, hormone therapy and radiotherapy, the point prevalence had fallen further to a very striking 2%. Moreover, it was not just some psychometric quirk of the Hospital Anxiety and Depression Scale. Other psychometric tests, and structured clinical interviews using standardised psychiatric criteria, confirmed the low rate of morbidity.
So, by applying simple, obvious, but key, principles, following the diagnosis, and during and after treatment, these women were mentally healthier than they had been at the time of diagnosis, and they were healthier than previously studied community cohorts of women. These exciting data suggest that a great deal can be done to prevent the widely reported high rates of psychological and psychiatric morbidity.
Prevention is better that cure. But can we go even further? Can we positively improve quality of life? Apart from compassionate reasons, there is another reason why it might make sense to think about the stress levels of our patients. A large and burgeoning literature shows that certain types of stress, especially certain types of chronic stress, have predictable effects on host defences, particularly by suppressing natural killer (NK) cell activity (Gruzelier, Clow, Evans, et al., 1998; Walker, 1999; Walker & Eremin, 1995).
We had previously shown in healthy volunteers (Johnson, Walker, Whiting, et al., 1996), and Professor Fawzy at the University of California in Los Angeles had shown in patients with melanoma (Fawzy, Cousins, Fawzy, et al., 1990; Fawzy, Kemeny, Fawzy, et al., 1990), that a psychological intervention could offset stress-induced immunosuppression. We should not be surprised by this. The brain is 'hard-wired' to the autonomic nervous system and the endocrine system, and these systems are known to play a part in the modulation of host defences. It is clear that the brain can communicate with host defences via these and other less well-defined pathways. It is not surprising, therefore, that what happens in the brain, particularly in the frontal lobes, in the limbic system and in the hypothalamus, can alter host defences (Walker, 2000).
For some types of cancer,there is clear evidence that immunosuppression affects clinical outcome. This slide summarises the main anti-tumour mechanisms in vivo. I would like to draw your attention to T-cell killing and natural cytotoxicity. Natural cytotoxicity includes natural killer (NK) cells and lymphokine activated killers (LAK) cells. Later this evening, I shall be presenting results of the effect of an intervention on various T cell subsets and on natural cytotoxicity. Meantime, it is important to note that these are thought to be important in terms of controlling, destroying and preventing the spread of some types of cancer. Here is an animation of NK cells in action.
Two NK cells have seen a cancer cell. They are attracted towards it chemotactically and, in the presence of calcium ions, they secrete a substance called perforin which punctures the cancer cell wall causing the cell to leak and to die.
For biological reasons, as well as from compassion, therefore, we want to improve the quality of life of our patients. We want to help patients to cope. We want to prevent stress-induced immunosuppression.
The psychoneuroimmunological effects of a simple intervention
We sought funding, therefore, from the Cancer Research Campaign to evaluate the effects of a simple intervention designed to reduced stress and to teach patients a method of feeling more in control. The main outcomes were quality of life, mood, coping, host defences and response to chemotherapy (Walker, Walker, Ogston, et al., 1999) .
This slide shows the overall trial design. Patients received cyclophosphamide, vincristine, adriamycin and prednisolone, six cycles every three weeks, followed by surgery, breast conservation or mastectomy, depending on the woman's preference and what was surgically feasible. Then, the women received 20 fractions of radiotherapy over a period of 4 weeks, and they were followed up 4 weeks and 12 weeks after radiotherapy; a 37-week protocol in all. Blood samples were taken, and psychological tests were administered, at the time points indicated.
Following the diagnosis, with their written informed consent, the women were randomised to a high level of support in the Behavioural Oncology Unit, which I have already described this evening, or to a similar high level of support plus our experimental intervention, relaxation plus guided imagery.
The 'relaxation response' is the opposite of the 'fight-flight' response. If you have ever had a fright, perhaps a near miss in a car, or someone breaking into your house, you will have noticed that not only do you feel anxious. Your body changes in various ways; for example, your mouth goes dry, your respiration rate increases and you feel cold because your peripheral blood vessels have constricted. This is the fight-flight response. It, and its opposite the relaxation response, are integrated hypothalamic responses. The fight-flight response results from an increase in sympathetic autonomic nervous system tone: the relaxation response arises from an increase in parasympathetic tone.
In addition to these physiological changes, the relaxation response is associated with feelings of relaxation, calmness and confidence. Using live training, or audio cassette recordings, most people can learn to switch on the relaxation response, by thinking trigger words such as 'one, two, three, relax'.
Images are very powerful, are they not? Certainly, the advertising industry thinks so; the use of images in advertising is a multibillion pound industry. Images can elicit feelings and they can also change behaviour even if the new behaviour may be lethal. The great physicist Albert Einstein was well aware of the importance of imagination when he said: 'Imagination is more important then education.'
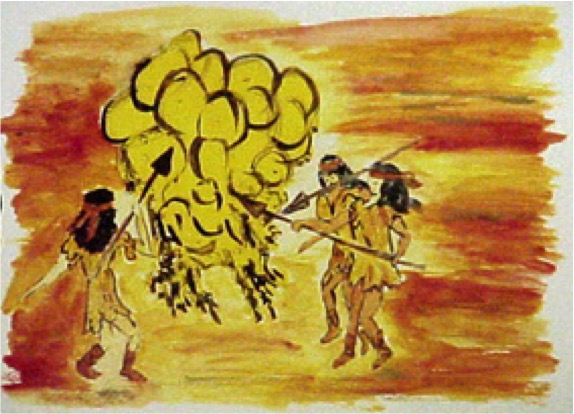
We issued our patients with a portfolio of 10 coloured cartoons as a resource. We also encouraged the women to develop their own images, and many of them did. One of our patients visualised three female warriors with spears attacking a large cluster of cancer cells. At a different stage in her treatment, she visualised a three-headed dragon breathing fire.
At baseline, we carried out a comprehensive assessment of personality, coping, mood, mental state, quality of life and host defences. Our main measures of outcome were quality of life, mood, coping, host defences and response to chemotherapy.
Clinical and pathological assessments of the response of the tumour(s) to chemotherapy were as follows. Clinical response was assessed after six cycles using standard internationally recognised criteria (UICC). Pathological response was assessed post-surgically from the excised specimen using a previously published 1-5 scale.
Here is an example of someone who, unfortunately, did not show a response to chemotherapy. The histopathology before chemotherapy is on the left hand side of the slide: the histopathology after chemotherapy is shown on the right. Following chemotherapy, there are still viable tumour nests. In contrast, the next slide shows a patient who showed a complete pathological response to chemotherapy.
Ninety-six women with large, or locally advanced, breast carcinoma as defined in this slide were recruited.
And now, the results.
As expected, during chemotherapy women in the control group showed a significant decline in self-rated global quality of life. In contrast, those women randomised to relaxation and guided imagery showed a slight improvement in quality of life. Formal evaluation of these between group differences using analysis of variance shows the obvious; there is significant difference between these two groups.
Turning now to mood: the higher the score the better. In the control group, mood deteriorates during chemotherapy, whereas in the experimental group it improves quite dramatically.
Remember in my introductory remarks, I said that emotional suppression and social conformity were characteristics of the Type C personality? Emotional suppression, as assessed by the Courtauld Emotional Control scale (Watson & Greer, 1983), is stable, as it should be, in the control group. In the experimental group, however, women clearly became much more emotionally expressive. Similarly, the intervention modified social conformity as measured by the L scale of the Eysenck Personality Questionnaire (Eysenck & Eysenck, 1991). Social conformity was relatively stable in the control group, whereas there was a progressive decline in the experimental group. These data show that the experimental intervention had a significant effect on important coping strategies.
The next slide shows the results for clinical and pathological response to chemotherapy. The two groups did not differ significantly in terms of either clinical or pathological response. However, using logistic regression and multiple regression, two independent predictors of chemotherapy response were discovered. These were tumour size at diagnosis, and mood disturbance at diagnosis. The larger the tumour, the poorer the response. The greater the mood disturbance at diagnosis, the poorer response (Walker, Walker, Ogston, et al., 1999).
To summarise, the psychological effects of relaxation and guided imagery included improved mood and quality of life and enhanced coping. The intervention did not affect response to chemotherapy, although mood disturbance was a significant independent predictor of a poor clinical response and a poor pathological response to chemotherapy.
The next slide shows the effect of relaxation and guided imagery on one parameter of host defences, namely activated (CD25+) T cells. The solid line represents the control group; the dotted line represents the experimental group. The vertical bars indicate one standard error, and the graph shows the mean numbers of CD25+ cells at various time-points during the 37-week protocol. More or less all the way through, those randomised to the experimental group have more activated T cells than those in the control group (Ogston, Walker, Simpson, et al., 1997).
Time precludes a detailed analysis of the immunological data. However, to summarise, between-group analyses revealed that the intervention increased lymphokine activated killer (LAK) cell activity, and increased the total number of T cells (CD2+), mature T cells (CD3+) and activated T cells (CD25+). Also, the intervention reduced the circulating levels of tumour factor alpha (TNF-a). Within the experimental group, we were able to correlate the women's self reports of imagery vividness as recorded in their daily diaries with changes in LAK and NK cell activity during chemotherapy and at the final follow up time point. There was a high, positive and statistically significant correlation. The more vivid the imagery, the higher the NK and LAK cells activity after chemotherapy, and 12 weeks after completion of radiotherapy.
We concluded that relaxation and guided imagery improved key aspects of quality of life, and that there were statistically significant changes in host defences. However, we are not yet in a position to determine the clinical significance of these biological changes. Statistical and clinical significance are not the same, and only careful follow up will show whether these alterations in host defences will translate into something that is clinically meaningful in terms of tumour biology.
Organisation of Services: Implications for the NHS
If we put together these findings on the prevention of morbidity, and the enhancement of quality of life, what are the implications for the NHS? What should we be doing to provide the best possible service for our patients and their families?
As the Pro Vice-Chancellor said in his kind words of introduction, the National Director of Cancer, Professor Michael Richards, has identified four priority areas for the National Cancer Plan. Significantly, and I believe correctly, patient information, support and palliative care are one of these four priorities.
In my view, nationally, the big challenges and the big opportunities are to improve information and support; to prevent psychological morbidity; to improve quality of life, to deliver effective interventions, and to deliver evidence-based interventions equitably -regardless of social class, regardless of race, regardless of creed.
Before I came to Hull and the East Riding, a very valuable piece of research had been carried out locally under the aegis of the Cancer Service Project. Patients were asked to indicate what one thing they would wish to change about the way their cancer has been managed. Of the 120 respondents, 85% said there was at least one thing that they would wish to change. What do you think would be most commonly mentioned? Would it be the time taken to reach a diagnosis; would it be the toxicity of the treatment; would it be better information, or would it be better support?
The most commonly mentioned aspect, in fact, was better support. One in four (26%) said that they would wish to improve the support that they had received from the professional health care staff. Fifteen per cent wished for improved communication between professionals and between professionals and them. The same number, 15%, wanted the initial referral speeded up. This is interesting because the government has been taking an initiative nationally to speed up referrals. Doubtless, a good initiative. However, in this cohort of patients almost twice as many wished improved support compared with faster referral. Improving information per se was mentioned by only 12%.
Since moving to the East Riding, we have been trying to apply the principles that we worked out in the Aberdeen Behavioural Oncology Unit. We have established, therefore, an Oncology Health Centre at the Princess Royal Hospital (East Hull): another is due to open soon at Castle Hill Hospital (West Hull). In time, we wish to set up peripheral satellite Centres, with video links, throughout the East Riding.
There are two components to the concept of an Oncology Health Centre. The first component is the 'drop in' centre. This has an informal atmosphere and is staffed by specially trained behavioural oncology nurses who have back-up from clinical and health psychologists. The second component is a referral-based service, staffed by psychologists, a psychiatric specialist registrar and behavioural oncology nurses.
Currently, on average, 125 patients and relatives attend the Princess Royal Hospital Oncology Health Centre: indeed, recently the weekly attendance topped 150. The Centre is open to all patients with cancer who are receiving, or have received cancer treatment locally. It is also open to their relatives. We try to make the Centre very informal and relaxed. There is drop in access to accurate information and support because we have available instantly the patient's records and the most up to date correspondence (on computer). Unlike some centres in other parts of the country we do not stand alone; we work hard at being fully integrated with the radiographers, with the medical oncologists, with the surgical oncologists, with the specialist nurses and with community agencies.
Moreover, we do not have, nor do we wish to have, a corner on the market: we see ourselves as being complementary to the very valuable work done by other members of the cancer team who provide support and information.
Here is snap shot of the Oncology Health Centre and also the front cover of our leaflet that we hope will be given to every new patient. 'Just drop in; can we help you?' Our mission statement, along with all the other professionals involved in cancer care, is to prevent distress; to enhance quality of life; to offer evidence-based interventions, and to give advice, support and supervision to staff. I was delighted when, within a few weeks of coming to Kingston upon Hull, I was approached by several groups of local nurses who wished me to set up regular supervision groups so that they could discuss important matters of clinical and organisational concern.
Already we have begun a training programme locally, and next year we are going to launch a national training programme. In addition, the Oncology Health Centres, of course, will provide us with our research infrastructure. In collaboration with clinicians and basic scientists, locally and elsewhere, we are planning new studies in psychoneuroimmunology, the development and evaluation of novel interventions, including complementary interventions, the psychosocial impact of screening and the evaluation of different models of service delivery.
We recently asked a consecutive series of patients who had visited the centre at least once to complete anonymously a satisfaction questionnaire. Interestingly, 100% of our patients and relatives agreed to do this: no one refused. Fifty-one patients and 38 relatives - 34 males and 55 females - responded. On average, they had visited the centre seven times (range 2-20).
They were asked to indicate on a Likert scale the extent to which they agreed or disagreed with various propositions:
- 100% agreed that 'Overall, I am satisfied with the care I have received in the Oncology Health Centre'.
- 100% agreed that 'I received a warm welcome.'100% agreed that 'The staff understood my concerns'.
- 100% agreed that 'The staff understood my concerns'.
- 100% agreed that 'The staff responded helpfully to my concerns'.
- 100% agreed that 'I found it useful to talk to with the nurses in the centre'.
- 100% agreed that 'I feel the doctors and nurses in the Oncology Health Centre provide a valuable service'.
- 100% agreed that 'I consider the Oncology Health Centre provides a unique dimension of care'.
- 96% agreed that 'I found it useful to talk with other patients'.
We also sent an anonymous questionnaire to all those who had referred one or more patients to the Oncology Health Centre. When I analysed the data two weekends ago, at that point we had received 38 replies. These 38 referrers had referred 369 patients: a mean of 9.7 patients with a range of 1-50. Most of the referrers were hospital nurses followed closely by physicians, then surgeons, other medics, community nurses and PAMS. The responses were as follows:
- 100% of our referrers felt that the centre made a useful contribution to the overall care.
- 100% felt it made a useful contribution to the welfare of relatives.
- 97% felt that what we did in the centre was unique.
- 100% were satisfied with speed of response and documentation.
- 97% were satisfied with communication and clinical outcome.
These audit data indicate that referrers, patients and relatives value the service very positively. Moreover, it is clear that the number of referrals and drop-ins is continuing to increase.
We are very grateful indeed for the continuing support of the local oncological community, both in hospital and in the community. Without that support, the Oncology Health Centre could not function properly.
I should also like to take this opportunity to say publicly how extremely fortunate I am in having such able, dedicated and enthusiastic colleagues in the Centre.
Psychosocial interventions and survival
Finally, psychosocial interventions and survival. We have seen that psychosocial interventions can enhance quality of life. But do psychosocial interventions make a difference to life expectancy?
As I said in my introductory remarks, the only way to be sure about this issue is to rely on the results from prospective, randomised, clinical trials -the gold standard for evaluating new treatments with drugs, complementary interventions or psychotherapy (Walker & Anderson, 1999).
Although a number of negative studies have been reported, there are four positive studies (Anderson & Walker, In press; Walker, Heys & Eremin, 1999) :
- 86 patients with metastatic breast cancer (Spiegel, Bloom, Kraemer, et al., 1989),
- 68 patients malignant melanoma (Fawzy, Fawzy, Hyun, et al., 1993)
- 94 patients with haematological malignancies (Richardson, Shelton, Krailo, et al., 1990)
- 63 patients with lymphoma (Walker, Ratcliffe & Dawson, 2000).
Let me expand on the results of our study. Sixty-three patients with Hodgkin's disease or non-Hodgkin's lymphoma were randomised to one of three interventions: (1) training in progressive muscular relaxation and cue controlled relaxation, (2) relaxation plus hypnotherapy (direct hypnotic suggestion, a novel technique that I called nausea management training and ego strengthening) or (3) standard treatment. The purpose of these was, in addition to antiemetic drugs, to reduce the severity and prevalence of chemotherapy side effects (nausea, vomiting and anticipatory anxiety) (Walker, 1992; Walker, Dawson, Pollet, et al., 1988).
Almost a year ago we completed our most recent follow up - the median time from diagnosis was 13 years and 5 months. We analysed the data using univariate (Log-rank test) and multivariate (Cox proportional hazards) methods.
Thirty-seven percent of the patients randomised to standard treatment compared with exactly 50% of those randomised to relaxation with, or without, hypnotherapy were still alive. The median survival of those in the standard treatment group was 74 months compared with a median survival of 115 months in those randomised to relaxation with, or without, hypnotherapy.
When those who had survived were compared one variable at a time with those who had died (univariate analysis), those who had died were older; they had more advanced disease at diagnosis, and they were more likely to have non-Hodgkin's lymphoma. This is unsurprising and reassuring. In addition, however, the social conformity, and depression scores on the Hospital Anxiety and Depression Scale, were also significant. On this univariate analysis, however, the effect of the intervention was not statistically significant.
The problem with univariate analyses is that the different variables are often themselves intercorrelated: what we really want to find out is which variables are genuinely independent predictors of survival. Using a very conservative form of multivariate analysis - Cox proportional hazards: simultaneous entry - the intervention now has a statistically significant effect on survival, along with stage of disease, depression and social conformity.
When we divided the patients into three groups according to their scores on social conformity (L scores), the Kaplan-Myer survival curves showed a most interesting pattern. The intervention clearly had no effect on survival on the low scorers. The curves for the middle third of scorers are beginning to look encouraging. However, when we look at the top scorers (7 or above), there is a highly statistically significant effect. All of those in the control group were dead by 2 years, whereas over 30% of those in the experimental group were still alive after 13 years (Walker, Ratcliffe & Dawson, 2000). These results were even more striking than they had been when we carried out a 5-years follow-up (Ratcliffe, Dawson & Walker, 1995).
Overall then, the interventions prolonged survival. In addition, social conformity, mood disturbance and stage at diagnosis were independent prognostic factors for survival. Sub-group analyses showed that the survival advantage was related to social conformity scores. High scorers benefited most from the interventions.
Now how might this come about? By what mechanisms might a psychosocial intervention prolong survival? There are several possibilities.
- Because of treatment side effects, some patients decide not to persevere with life-prolonging, or even curative, treatments. However, there is evidence that psychological interventions can improve treatment compliance (Richardson, Shelton, Krailo, et al., 1990). The first patient whom I ever saw with cancer was one such individual. She had curable Hodgkin's disease and was refusing further chemotherapy because the side effects were so severe. With the help of a novel intervention, she was able to complete successfully her prescribed course of chemotherapy (Walker, 1985; Walker, Dawson, Pollet, et al., 1988).
- Whether or not you have cancer, adopting a healthy lifestyle is likely to be beneficial. Interventions may encourage such a life-style.
- In our breast cancer study, we found that mood disturbance predicted poorer clinical and pathological responses to chemotherapy via an as yet undefined mechanism. Psychosocial interventions may affect survival by improving mood, thereby improving response to chemotherapy.
- We have shown that interventions have measurable effects on host defences, and there is reason to believe that they also affect hormones, etc. To the extent that host defences and hormones are relevant to tumour progression, interventions may influence survival through these pathways.
- Finally, a small, but significant, number of patients develop serious infectious complications during chemotherapy. If interventions can prevent or ameliorate some of the chemotherapy-induced immunosuppression, they may reduce the number of associated deaths from neutropenic sepsis (Walker, 2000).
I believe that further work is required to determine which patients (in terms of personality, type of cancer, stage at presentation) might benefit from particular interventions via specific mechanisms. At this stage we must be cautious. Although the data are immensely exciting, they are inconclusive. We must be careful not to raise expectations unrealistically. We must conclude that, at the present time, a beneficial effect of psychosocial interventions on recurrence and survival is not yet proven.
Conclusions
Pro Vice-Chancellor, Ladies and Gentlemen, the biopsychosocial approach to cancer that I have described this evening holds out the promise of profound new insights into the malignant process and cancer therapeutics. If future studies confirm that psychosocial interventions not only improve quality of life, but also significantly prolong survival, that will be a huge bonus.
However, we must not sit back and wait for these studies. If we apply even a fraction of the evidence that has accrued over the past two decades, we can say with certainty that a great deal can be done to prevent distress and to enhance quality of life following the diagnosis of cancer -not in ten years; not in five years; not even next year. By applying what we have already learned, undoubtedly, we can improve the lives of our patients and their families - now!
Thank you all very much for coming; and thank you all very much for listening so attentively.
References
Anderson, J. & Walker, L. G. (In press) Psychological factors and
cancer progression: involvement of behavioural pathways. In The
Psychoimmunology of Cancer (eds C. E. Lewis, R. O'Brien & J.
Barraclough), Second Edition. Oxford: Oxford University Press.
Anderson, J., Walker, M. B. & Walker, L. G. (2000) Distress and concerns
of the partners of patients with breast cancer who receive primary
chemotherapy. Psycho-Oncology, 9, 357.
Bahnson, C. B. (1980) Stress and cancer: the state of the art (part 2).
Psychosomatics, 22, 202-220.
Derogatis, L. R., Morrow, G. R., Fetting, J., et al (1983) The
prevalence of psychiatric disorders among cancer patients. Journal of
the American Medical Association, 249 (6), 751-7.
Eysenck, H. J. & Eysenck, S. B. G. (1991) Manual of the Eysenck
Personality Scales (EPS Adult). London: Hodder and Stoughton.
Fawzy, F. I., Cousins, N., Fawzy, N. W., et al (1990) A structured
psychiatric intervention for cancer patients. I. Changes over time in
methods of coping and affective disturbance. Archives of General
Psychiatry, 47, 720-5.
Fawzy, F. I., Fawzy, N. W., Hyun, C. S., et al (1993) Malignant
melanoma. Effects of an early structured psychiatric intervention,
coping, and affective state on recurrence and survival 6 years later.
Archives of General Psychiatry, 50, 681-9.
Fawzy, F. I., Kemeny, M. E., Fawzy, N. W., et al (1990) A structured
psychiatric intervention for cancer patients. II. Changes over time in
immunological measures. Archives of General Psychiatry, 47,
729-35.
Greer, S., Morris, T., Pettingale, K. W., et al (1990) Psychological
response to breast cancer and 15-year outcome. Lancet, 335 (8680),
49-50.
Gruzelier, J., Clow, A., Evans, P., et al (1998) Mind-body
influences on immunity: lateralised control, stress, individual
difference predictors and prophylaxis. Annals of the New York Academy of
Science, 851, 487-494.
Harrison, J. and Maguire, P. (1994). Predictors of psychiatric morbidity
in cancer patients. British Journal of Psychiatry, 165, 593-598.
/>
Johnson, V. C., Walker, L. G., Whiting, P. H., et al (1996) Can
relaxation training and hypnotherapy modify the immune response to acute
stress, and is hypnotisability relevant? Contemporary Hypnosis, 13,
100-108.
Klein, S., Kitchener, H. C., Tracy, D., et al (2000) The effects of
cancer patient participation in teaching communication skills to medical
undergraduates: a follow-up evaluation. European Journal of Cancer,,
36, 273-281.
Maguire, G. P., Lee, E. G., Bevington, D. J., et al (1978) Psychiatric
problems in the first year after mastectomy. British Medical Journal, 1
(6118), 963-5.
Maguire, G. P., Tait, A., Brooke, M., et al (1980) Psychiatric morbidity
and physical toxicity associated with adjuvant chemotherapy after
mastectomy. British Medical Journal, 281 (6249), 1179-80.
Ogston, K., Walker, M. B., Simpson, E., et al (1997) A controlled
clinical trial of the immunological effects of relaxation training and
guided imagery in women with locally advanced breast cancer. European
Journal of Surgical Oncology, 23, 372.
Paraskevaidis, E., Kitchener, H. C. & Walker, L. G. (1993)
Doctor-patient communication and subsequent mental health in women
with gynaecological cancer. Psycho-Oncology, 2, 195-200.
Pettingale, K. W., Morris, T., Greer, S., et al (1985) Mental attitudes
to cancer: an additional prognostic factor. Lancet, 1 (8431), 750.
Ratcliffe, M. A., Dawson, A. A. & Walker, L. G. (1995) Eysenck
Personality Inventory L-scores in patients with Hodgkin's
disease and non-Hodgkin's lymphoma. Psycho-Oncology, 4,
39-45.
Richardson, J. L., Shelton, D. R., Krailo, M., et al (1990) The effect
of compliance with treatment on survival among patients with hematologic
malignancies. Journal of Clinical Oncology, 8, 356-64.
Spiegel, D., Bloom, J. R., Kraemer, H. C., et al (1989) Effect of
psychosocial treatment on survival of patients with metastatic breast
cancer. Lancet, 2 (8668), 888-91.
Temoshok, L. (1985) Bio-psychosocial studies in cutaneous malignant
melanoma: Psychosocial factors associated with prognostic indicators,
progression, psychophysiology and tumour-host response. Social
Science and Medicine, 20, 833-840.
Walker, L. G. (1985) Aversions to chemotherapy in patients with lymphoid
tumours. In Proceedings, First Annual Conference, British Society for
Experimental and Clinical Hypnosis (ed M. Heap), pp. 86-91. London:
BSECH Publications.
Walker, L. G. (1992) Hypnosis and cancer. American Journal of Preventive
Psychiatry and Neurology, 3, 42-49.
Walker, L. G. (1996) Communication skills: when, not if, to teach.
[editorial]., European Journal of Cancer, 32A, 1457-1459.
Walker, L. G. (1999) Psychological interventions, host defences and
survival. Advances in Mind-Body Medicine, 15, 236-281.
Walker, L. G. (2000) The psychoimmunology of cancer. Cancer Topics, 11
(17-19).
Walker, L. G. & Anderson, J. (1999) Testing complementary and
alternative therapies within a research protocol. European Journal of
Cancer, 35, 1614-1618.
Walker, L. G., Dawson, A. A., Pollet, S. M., et al (1988) Hypnotherapy
for chemotherapy side effects. British Journal of Experimental and
Clinical Hypnosis, 5, 79-82.
Walker, L. G. & Eremin, O. (1995) Psychoneuroimmunology: a new fad or
the fifth cancer treatment modality? [editorial]. American Journal of
Surgery, 170, 2-4.
Walker, L. G., Heys, S. D. & Eremin, O. (1999) Surviving cancer: do
psychosocial factors count? [editorial]. Journal of Psychosomatic
Research, 47, 497-503.
Walker, L. G., Ratcliffe, M. A. & Dawson, A. A. (2000) Relaxation and
hypnotherapy: long term effects on the survival of patients with
lymphoma. Psycho-Oncology, 9, 355-356.
Walker, L. G., Walker, M. B., Ogston, K., et al (1999) Psychological,
clinical and pathological effects of relaxation training and guided
imagery during primary chemotherapy. British Journal of Cancer, 80,
262-8.
Watson, M. & Greer, S. (1983) Development of a questionnaire measure of
emotional control. Journal of Psychosomatic Research, 27,
299-305.
Worden, J. W. and Weisman, A. D. (1984). Preventative psychosocial
intervention with newly diagnosed cancer patients. General Hospital
Psychiatry, 6, 243-249.
Zigmond, A. S. & Snaith, R. P. (1983) The Hospital Anxiety and
Depression Scale. Acta Psychiatrica Scandinavica, 67, 361-367.